Procedures
Cervical/Neck
- Posterior Cervical Laminectomy and Fusion

Posterior cervical fusion (PCF), a surgical procedure performed through the back of the neck, involves joining or fusing two or more damaged cervical vertebrae.
Know More - Cervical Corpectomy and Strut Graft
A cervical corpectomy and strut graft is a surgical procedure aimed at relieving the compression on the spinal cord by removing the degenerated vertebrae and replacing them with a bone graft.
Know More - Cervical Laminoplasty

A cervical laminoplasty is an operative procedure that involves reshaping/repositioning the bone at the neck region (cervical spine) to relieve excess pressure on the spinal nerves.
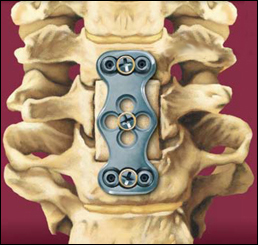
Know More - Anterior Cervical Discectomy with Fusion

Anterior cervical discectomy with fusion is an operative procedure to relieve compression or pressure on nerve roots and/or the spinal cord due to a herniated disk or bone spur in the neck.
Know More Launch Movie - Artificial Cervical Disk Replacement

Artificial cervical Disk replacement is a spine surgery to replace a degenerated (deteriorated) Disk in the neck with an artificial Disk.
Know More Launch Movie - Cervical Foraminotomy

Cervical foraminotomy is a surgical procedure performed to relieve the symptoms of a pinched or compressed spinal nerve by enlarging the neural foramen, an opening for the nerve roots to exit the spine and travel through the body.
Know More
Thoracic/Lumbar
- Lumbar Laminectomy

Lumbar laminectomy, also known as decompression laminectomy, is a spinal surgery performed to relieve excess pressure on the spinal nerve(s) in the lumbar (lower back) region.
Know More - Posterior Lumbar Fusion

Lumbar fusion is the fusion the vertebrae in the lumbar portion of the spine (lower back).
Know More Launch Movie - Anterior Lumbar Interbody Fusion

Anterior lumbar interbody fusion (ALIF) is a surgery performed to correct spinal problems in the lower back. The surgery can be implemented either as an open surgery or minimally invasive technique.
Know More Launch Movie - Surgery for Scoliosis

Surgery for scoliosis is recommended when the spinal curvature is severe and is either worsening or is a cause of severe pain or difficulty in breathing.
Know More
Minimally Invasive Surgery
- Lumbar Endoscopic Discectomy
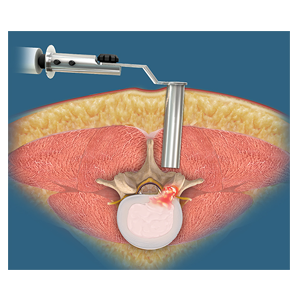
Lumbar endoscopic discectomy is a minimally invasive surgical procedure to treat a herniated or ruptured disk and relieve pressure on the spinal nerves.
Know More - Minimally Invasive Lumbar Discectomy
A lumbar discectomy is a surgical procedure performed to treat a herniated or ruptured disk and relieve pressure on the spinal nerves.
Know More - Minimally Invasive TLIF

Transforaminal lumbar interbody fusion (TLIF) is a minimally invasive fusion of the vertebrae of the lumbar region (lower back). It is designed to provide stability to the spine and treat back and leg pain.
Know More Launch Movie - Kyphoplasty

Balloon kyphoplasty is a spine surgery that relieves back pain caused by a vertebral compression fracture. The aim of balloon kyphoplasty is to relieve pain, stabilize the fracture and restore the vertebral body height.
Know More - Minimally Invasive Spine Surgery

Minimally invasive spine surgery (MISS) is the latest technology available to perform spinal surgeries through small, less than one-inch-long incisions.
Know More - Oblique Lumbar Interbody Fusion (OLIF)

Oblique lumbar interbody fusion (OLIF) is a minimally invasive approach to LIF, where an incision is made on your side to avoid damaging important muscles and ligaments in your back.
Know More - Endoscopic Spine Surgery

Endoscopic spine surgery is a minimally invasive spine surgery that uses specialized video cameras and instruments to remove the herniated disk through very small incisions.
Know More - Image-Guided Spine Surgery

Imaging techniques such as computed tomography and fluoroscopy may be integrated into the system to facilitate pre-operative planning of the surgery...
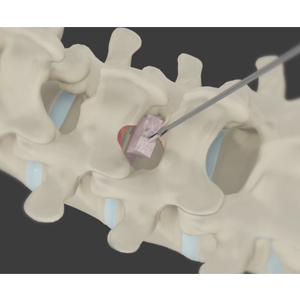
Know More - Extreme Lumbar Interbody Fusion (XLIF)

Extreme lumbar interbody fusion (XLIF) or direct lateral interbody fusion (DLIF) is a surgical procedure indicated in various spine conditions.
Know More Launch Movie
