Lumbar Endoscopic Discectomy
Disease Overview
The lower back or lumbar region is often the site of pain due to its high mobility and weight bearing. Spongy disks present between the vertebral bones helps cushion the spine during stress and movement. The intervertebral disks in the lumbar region may get damaged due to stress, causing them to herniate or rupture, and compress on adjacent spinal nerves. This can lead to lower back pain, as well as pain, weakness, and numbness in the lower legs.
What is Lumbar Endoscopic Discectomy?
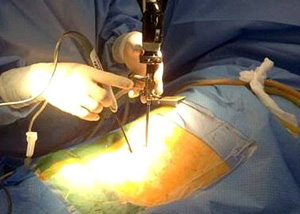
Lumbar endoscopic discectomy is a minimally invasive surgical procedure to treat a herniated or ruptured disk and relieve pressure on the spinal nerves.
Lumbar Endoscopic Discectomy Procedure
Lumbar endoscopic discectomy is performed under local anesthesia. With the help of imaging studies, your doctor identifies the affected disk and inserts a metal tube into the disk space. An endoscope, a lighted viewing tube with a camera, is introduced through the metal tube to enable your doctor to view enlarged live images on a monitor. Instruments are then introduced through the metal tube and the surgery performed under image guidance. The herniated or ruptured disk is removed and components placed to stabilize the spine.
Advantages of Lumbar Endoscopic Discectomy
Lumbar endoscopic discectomy is a minimally invasive procedure that usually results in lower blood loss, less pain, minimal tissue damage, shorter hospital stay, and a faster recovery.
Risks and Complications of Lumbar Endoscopic Discectomy
Though complications are rare, lumbar endoscopic discectomy may be associated with prolonged pain, infection, bleeding, nerve injury and spinal fluid leakage.
- Postoperative Protocol
- Prof. Daniel Park highlights benefits of biportal endoscopic spine surgery
- Case Study
Related Topics:
- Lumbar Laminectomy
- Posterior Lumbar Fusion
- Lumbar Endoscopic Discectomy
- Minimally Invasive Lumbar Discectomy
- Anterior Lumbar Interbody Fusion
- Minimally Invasive TLIF
- Kyphoplasty
- Minimally Invasive Spine Surgery
- Oblique Lumbar Interbody Fusion (OLIF)
- Posterior Cervical Laminectomy and Fusion
- Cervical Corpectomy and Strut Graft
- Endoscopic Spine Surgery
- Surgery for Scoliosis
- Cervical Laminoplasty
- Image-Guided Spine Surgery
- Anterior Cervical Discectomy with Fusion
- Artificial Cervical Disk Replacement
- Cervical Foraminotomy
- Extreme Lumbar Interbody Fusion
